With the development of critical care, more people are now surviving critical illness. The task of healthcare professionals and researchers is to discover how to help these patients recover and regain the best quality of life they can after the ICU. ICU recovery programs are essential as they address various challenges that arise after intensive care, including physical, cognitive, and psychological impairments. This article explores the key components, implementation strategies, outcomes, and future directions of ICU recovery programs, backed by recent research findings.
The Need for Recovery Programs
As ICU survival rates improve, we’re getting more familiar with long-term consequences of critical illness collectively known as Post-Intensive Care Syndrome (PICS). PICS represents a wide range of physical, cognitive and psychological issues that can affect more than half of ICU survivors1Tejero-Aranguren, J., Martin, R. G. D. M., Poyatos-Aguilera, M. E., Morales-Galindo, I., Cobos-Vargas, A., & Colmenero, M. (2022). Incidence and risk factors for post-intensive care syndrome in a cohort of critically ill patients. Revista Brasileira de Terapia Intensiva, 34, 380-385.2Yuan, C., Timmins, F., & Thompson, D. R. (2021). Post-intensive care syndrome: a concept analysis. International journal of nursing studies, 114, 103814.. These challenges necessitate structured recovery programs to facilitate rehabilitation and support for patients transitioning from hospital to home.
Key Components of Successful ICU Recovery Programs
Research3McPeake, J., Boehm, L. M., Hibbert, E., Bakhru, R. N., Bastin, A. J., Butcher, B. W., … & Sevin, C. M. (2020). Key components of ICU recovery programs: what did patients report provided benefit?. Critical care explorations, 2(4), e0088. has identified five components that contribute to the effectiveness of ICU recovery programs:
- Continuity of Care: Many patients have reported that clinicians involved in post-ICU programs played a vital role in managing their ongoing medical needs, particularly for conditions that were not fully resolved before discharge. Fragmented care leads to communication gaps leaving patients feeling lost and unsupported, waiting for answers about their treatment, unsure of whom to contact for help. Continuity of care ensures that patients feel more connected and informed about their health status, leading to more effective management of their ongoing symptoms and a smoother transition back to everyday life.
- Improving Symptom Status: Patients often experience a range of new and ongoing symptoms after their ICU stay, which can include not only physical issues but also emotional and social challenges associated with PICS. To effectively manage these symptoms, it is crucial to integrate health and social care. Many patients highlighted the importance of linking them to community resources that address not just their medical needs but also their emotional and social well-being. Patients reported that creating accurate memories of their ICU experience helped reduce feelings associated with PTSD. This was achieved through direct answers to their questions from ICU staff and structured summaries like discharge letters or patient diaries that clarified their treatment journey.
- Normalization and Expectation Management: Educating patients about their recovery trajectory helps them set realistic goals and reduces anxiety about their future capabilities. This component emphasizes the importance of providing clear information about what to expect during recovery.
- Internal and External Validation of Progress: Regular feedback on recovery milestones helps patients recognize and appreciate their individual achievements during the rehabilitation process. This validation is crucial for staying motivated to keep participating in their rehabilitation process.
- Reducing Feelings of Guilt and Helplessness: Many ICU survivors experience guilt related to their condition or feelings of helplessness. Patients who did not have access to recovery programs frequently reported feeling helpless regarding their symptoms and the adjustments required to adapt to their “new normal.” They noted that targeted interventions aimed at helping both patients and caregivers could alleviate feelings of guilt.
Implementation Strategies
Implementing effective ICU recovery programs requires a multidisciplinary approach:
- Early Involvement: Starting discussions about recovery while patients are still in the ICU can help set the stage for successful transitions. Helping patients set goals from the start can help them take ownership of their recovery journey4Boehm, L. M., Danesh, V., Eaton, T. L., McPeake, J., Pena, M. A., Bonnet, K. R., … & Sevin, C. M. (2023). Multidisciplinary ICU recovery clinic visits: a qualitative analysis of patient-provider dialogues. Chest, 163(4), 843-854.
- Multidisciplinary Teams: A collaborative5Meyer, J., Slack, A., Waldmann, C., Bastin, A., Gager, M., McPeake, J., … & Wilson, E. (2021). Life after critical illness: a guide for developing and delivering aftercare services for critically ill patients. approach involving various healthcare professionals—physicians, nurses, physiotherapists, psychologists—helps cover all parts of the recovery.
Telemedicine: Using telemedicine during recovery for follow-up appointments ensures easier access to care, from anywhere, any time when patients are in need.
Outcomes of ICU Recovery Programs
Evidence suggests that participation in structured ICU recovery programs leads to significant improvements in quality of life for survivors. Research indicates that these programs can reduce symptoms of post-traumatic stress disorder (PTSD) and depression while enhancing overall mental health outcomes6Rosa R.G., Ferreira G.E., Viola T.W., et al. Effects of post-ICU follow-up on subject outcomes: a systematic review and meta-analysis. J Crit Care. 2019;52:115–125. doi: 10.1016/j.jcrc.2019.04.014. Additionally, patients report feeling more empowered and engaged in their care when they receive consistent support from healthcare providers.
More research is needed to determine the exact structure of ICU programs that leads to the best outcomes for patients. Additionally, more support and funding is needed for this research and ultimately, country-wide implementation.
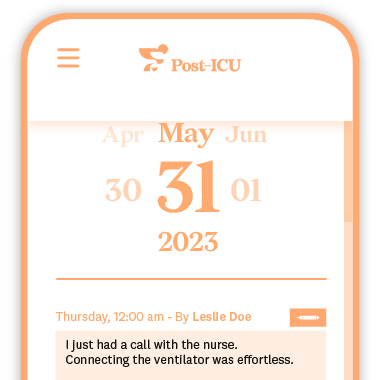
Post-ICU Digital Diary: A Tool for Successful ICU Recovery
ICU recovery programs play a crucial role in addressing the complex needs of patients after critical illness. Having a complete picture of what happened during ICU stay helps patients process and cope with the psychological trauma they experienced. A digital tool such as the Post-ICU diary serves as a therapeutic resource, allowing patients and their families to document their experiences, thoughts, and feelings during and after their ICU stay. As healthcare systems continue to evolve, prioritizing structured recovery initiatives will be essential in ensuring that patients not only survive but thrive following their ICU experiences.