Delivering effective healthcare while maintaining financial sustainability presents a challenge many ICUs in the US face. Advancements in science, technology, and medical capabilities are making the delivery of critical care more complex than ever increasing error potential and inconsistent quality care. This is why maximizing efficiency in the ICU is paramount.
Highly efficient ICUs show optimal use of resources, defined and streamlined processes to deliver high-quality care to critically ill patients. It involves maximizing productivity and reducing wastage which leads to higher staff and patient satisfaction as well as better clinical outcomes.
In this article, we have identified seven key areas within ICUs where efficiency improvements can be made, as well as explored practical strategies to achieve that.
Why Is Efficiency in the ICU Important?
Reduce the Potential for Error
Many studies suggest that the potential for error in the ICU is increased by communication problems1Donchin, Y., Gopher, D., Olin, M., Badihi, Y., Biesky, M., Sprung, C., Pizov, R., & Cotev, S. (1995). A look into the nature and causes of human errors in the intensive care unit*. Quality and Safety in Health Care, 12, 143 – 147, the complexity of patient care2Nichter, M. (2008). Medical errors affecting the pediatric intensive care patient: incidence, identification, and practical solutions.. Pediatric clinics of North America, 55 3, 757-77, xii), the high number of medications prescribed3Kane-Gill, S., & Weber, R. (2006). Principles and practices of medication safety in the ICU.. Critical care clinics, 22 2, 273-90, vi, characteristics of the ICU environment4Donchin, Y., & Seagull, F. (2002). The hostile environment of the intensive care unit. Current Opinion in Critical Care, 8, 316-320. such as complicated devices and ambient factors, and specific patient factors like gender and acuity level.
Patient Outcomes
Multiple studies show that efficient ICU operations can lead to better patient outcomes. By streamlining processes, reducing delays, and minimizing errors, patients receive timely and appropriate care, which can improve their chances of recovery and survival5Nguyen, Y. L., Wunsch, H., & Angus, D. C. (2010). Critical care: the impact of organization and management on outcomes. Current opinion in critical care, 16(5), 487-492..
Cost Reduction
Although ICU beds comprise less than 10% of hospital beds, ICU departments consume up to 22% of total hospital costs in the United States6ICU Beds Market Size, Growth Revenue, Industry Analysis, Overview By 2033. (n.d.). https://www.thebusinessresearchcompany.com/report/icu-beds-global-market-report#:~:text=Critical%20care%20is%20often%20described,bed%20in%20a%20general%20ward. Inefficient ICU operations can lead to unnecessary expenses, including overtime costs, extended lengths of stay, and avoidable complications. Increasing efficiency helps hospitals reduce costs while maintaining or even improving the quality of care provided.
Staff Satisfaction and Burnout Prevention
ICU staff dissatisfaction and burnout7Embriaco, N., Papazian, L., Kentish-Barnes, N., Pochard, F., & Azoulay, E. (2007). Burnout syndrome among critical care healthcare workers. Current opinion in critical care, 13(5), 482-488. are in part due to ICU organization. Efficient workflows reduce unnecessary stress and workload on ICU staff, leading to higher job satisfaction and lower rates of burnout. This, in turn, can improve staff retention and morale, ultimately benefiting both patients and healthcare organizations.
How to Measure ICU Efficiency?
Standardized mortality rate (SMR) and standardized resource use (SRU) are measures of efficiency in ICUs8Rothen, H. U., Stricker, K., Einfalt, J., Bauer, P., Metnitz, P. G., Moreno, R. P., & Takala, J. (2007). Variability in outcome and resource use in intensive care units. Intensive care medicine, 33, 1329-1336.. With ICU care costs on the rise, assessing performance should consider both clinical outcomes and resource use. One such measure is the Standardized Resource Use (SRU), which factors in total hospitalization and ICU stay adjusted for patient severity. An SRU above one (SRUR >1.0) indicates higher resource use than expected, while below one (SRUR <1.0) suggests efficient resource allocation.
It’s best interpreted alongside the Standardized Mortality Ratio (SMR) to understand the efficiency in resource utilization and clinical outcomes.
Ways to Increase Efficiency in the ICU
1. Foster a Culture of Continuous Improvement and Embracing Change
Introducing changes to improve ICU efficiency won’t be possible unless there’s a culture that accepts these changes. Here are the best practices to achieve that:
- Set clear priorities and focus on a select few initiatives so the ICU staff can commit to seeing them through rather than being overwhelmed by multiple changes
- Get buy-in from frontline staff to ensure they are driven, invested, and enthusiastic about the initiative. This can be done through the theory of “planned behavior” which means providing the critical care staff with evidence-based strategies they can implement in their day-to-day care delivery setting expectations of behaviors.
- Consider various types of incentives for compliance with the initiatives
Without the critical care staff on board, the initiatives may fall through and the hospital will lose valuable time and resources. Preparation and culture are key.
2. Implement Triage Protocols and Guidelines
Implementing triage protocols and guidelines can address existing inefficiencies9Cooke, C. R. (2013). Improving the efficiency of ICU admission decisions. Critical care medicine, 41(2), 662-663 in critical care services, which often lead to overuse and rising costs related to ICU admissions. Currently, regional differences in ICU admission rates primarily stem from the availability of ICU beds10Wennberg JE, Fisher ES, Stukel TA, et al: Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ 2004; 328:607, rather than variations in disease prevalence, severity, or patient preferences11Barnato AE, Herndon MB, Anthony DL, et al: Are regional variations in end-of-life care intensity explained by patient preferences?: A Study of the US Medicare Population. Med Care 2007; 45:386–393.
Triage protocols play a critical role in matching the demand for critical care with available resources. Without these protocols, there is a risk of admitting patients with low risk of death12Rosenthal GE, Sirio CA, Shepardson LB, et al: Use of intensive care units for patients with low severity of illness. Arch Intern Med 1998; 158:1144–1151 unnecessarily, while the “rule of rescue” may lead to the admission of terminally ill patients. Standardized guidelines for patient admission and discharge can streamline the admission process, ensuring that ICU resources are allocated efficiently and towards patients who can benefit from them the most.
Recommendations for effective triage protocols include:
- clear criteria for admission,
- regular review and updating of protocols based on patient outcomes,
- and involvement of multidisciplinary teams in decision-making processes.
By implementing these protocols, hospitals can optimize resource utilization in the ICU and improve patient outcomes.

Critical care triage protocol example (Source)
3. Improve Staff Communication and Collaboration
Improving team collaboration and communication is crucial for improving efficiency in ICU settings, and hospital managers can take several steps to achieve this.
Firstly, invest in strategies such as coaching and team building, drawing insights from business literature13Gershengorn, H. B., Kocher, R., & Factor, P. (2014). Management strategies to effect change in intensive care units: lessons from the world of business. Part III. Effectively effecting and sustaining change. Annals of the American Thoracic Society, 11(3), 454-457.. Experienced colleagues or formally trained peers can act as coaches or can provide valuable feedback and enhance clinical skills among staff. Organizations like the Society of Critical Care Medicine and government health departments offer coaching programs to support ICU care providers and hospital initiatives.
Secondly, recognize the importance of multidisciplinary ICU teams, which have been shown to improve protocol development, safe work environments, and hospital mortality rates. Keep in mind that perceptions of the current ICU climate and teamwork may vary among team members and managers. Therefore, you can target specific aspects such as leadership style, psychological safety, and mutual accountability to improve staff cohesion and efficiency.
Lastly, implementing team-building strategies like simulator training, classroom education, and facilitated group meetings can further enhance teamwork and communication within medical teams, ultimately improving efficiency in the ICU.
4. De-Siloed ICU for Increased Efficiency
Siloed thinking, common within hospital structures, can impede communication and collaboration, hindering quality, safety, and ultimately – efficiency.
Understanding that critical care extends beyond the ICU itself is crucial; patients often become critically ill outside the ICU, and fragmented care models can lead to conflicting understandings of care goals and resource allocation.
Implementing integrated management structures14Gershengorn, H. B., Kocher, R., & Factor, P. (2014). Management strategies to effect change in intensive care units: lessons from the world of business. Part III. Effectively effecting and sustaining change. Annals of the American Thoracic Society, 11(3), 454-457., such as service lines, can improve care coordination and streamline resource allocation across clinical scenarios and care phases.
Furthermore, unifying critical care under a single department or management can foster economies of scale, standardize care practices, and improve resource allocation across multiple ICUs within an institution.
5. Introduce Innovative Technologies to Increase Efficiency in the ICU
Technology affects ICU efficiency by automating processes, improving communication, and providing real-time data for informed decision-making. The type of technology you choose to introduce in your ICU will depend on the specific challenges your ICU staff is facing.
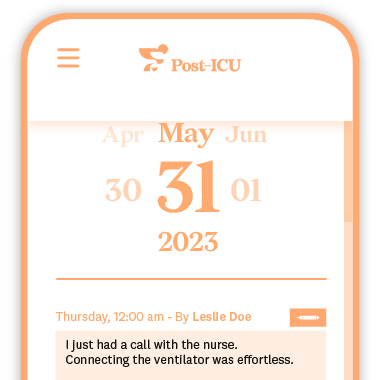
For example, streamlining workflow, reducing admin burden, and improving provider-patient communication all influence ICU efficiency. A tool like Post-ICU digital diary can help you tackle all three of these areas.
Post-ICU is a digital diary used by families of critically ill patients and the ICU staff (nurses) to record day-to-day social, sensory and visual occurrences. This helps ICU patients and family in their recovery phase to deal with anxiety, stress and prevent PTSD. In addition to benefiting patients and their families, the Post-ICU diary has been shown to streamline communication and reduce the time nurses spend providing updates to families of patients, allowing them more time to focus on patient care.
Discover how Griffin Hospital increased their ICU patient experience effectively with Post-ICU.
Some other examples of technology used in the ICU are:
- Electronic Health Records (EHRs) – data analysis and patient monitoring within the ICU for efficient data management, better communication between clinicians and avoiding errors
- Computerized Physician Order Entry (CPOE) – electronic prescribing of medications and ordering of tests, for legible orders, faster completion, inventory management, and automatic billing
- TeleICU – extend critical care, improve compliance, and facilitate transfers, through remote consultations, education, and monitoring.
6. Streamlining Workflow and Processes
Identifying bottlenecks and inefficiencies in ICU workflow is crucial for improving efficiency and patient care. This involves analyzing each step of the workflow to pinpoint areas where delays or inefficiencies occur, such as patient admission, discharge, or transfer processes.
Here are several ways to streamline processes in the ICU
- value stream mapping – visualize and analyze the entire process of patient care delivery, from admission to discharge. By mapping out the flow of activities, resources, and information, teams can streamline processes, eliminate waste, and optimize resource utilization
- standardizing workflows – establishing consistent and efficient protocols, procedures, and best practices for various tasks and activities within the ICU. This ensures that all team members follow uniform processes, reducing variability, errors, and delays in patient care
- continuous improvement – regularly reviewing processes, gathering feedback from staff and patients, and making small changes over time help teams continuously grow and improve
Various studies suggest that streamlining workflow in the ICU can be achieved through minimizing non-value-adding steps15Howell, M. (2011). Managing ICU throughput and understanding ICU census. Current Opinion in Critical Care, 17, 626–633., employing standard quality improvement practices, using EHR data and analytics16Ozkaynak, M., Dziadkowiec, O., Mistry, R., Callahan, T., He, Z., Davies, S., & Tham, E. (2015). Characterizing workflow for pediatric asthma patients in emergency departments using electronic health records. Journal of biomedical informatics, 57, 386-98, limiting interruptions17Giri, J., Ahmed, A., Dong, Y., Keegan, M., Herasevich, V., Pickering, B., & Gajic, O. (2013). Daily Intensive Care Unit Rounds: A Multidisciplinary perspective. Applied Medical Informatics, 33, 63-73., enhancing information transparency18Sanner, T., & Øvrelid, E. (2019). Informating Hospital Workflow Coordination. Computer Supported Cooperative Work (CSCW), 1-31., coordinating through dedicated roles and meetings, and implementing novel task management tools19Srinivas, P. (2015). Modeling Clinical Workflow in Daily ICU Rounds to Support Task-based Patient Monitoring and Care. Proceedings of the 18th ACM Conference Companion on Computer Supported Cooperative Work & Social Computing..
The ICU staff should be mindful of all these types of discomfort and be highly aware of how their actions impacts patients. For example, noise and light are high on the list of irritants20Tronstad, O., Flaws, D., Patterson, S., Holdsworth, R., & Fraser, J. F. (2023). Creating the ICU of the future: patient-centred design to optimise recovery. Critical Care, 27(1), 402. for ICU patients, and their effect can be directly exacerbated by the ICU staff.
Establish a warm and welcoming environment via providing positive distractions (e.g. music), intentional interactions with patients and their families, accessible amenities, etc.
7. Efficient and timely patient discharge
Achieving an optimal patient flow21van Sluisveld, N., Zegers, M., Westert, G., Van der Hoeven, J. G., & Wollersheim, H. (2013). A strategy to enhance the safety and efficiency of handovers of ICU patients: study protocol of the pICUp study. Implementation Science, 8, 1-9. is essential for maximizing ICU facility usage and maintaining quality care standards. Discharging patients helps alleviate pressure on ICU beds, but the risk of premature discharge must be cautiously managed to avoid premature or suboptimal discharges, resulting in ICU readmissions and potentially even patient fatalities22Chrusch, C. A., Olafson, K. P., McMillan, P. M., Roberts, D. E., & Gray, P. R. (2009). High occupancy increases the risk of early death or readmission after transfer from intensive care. Critical care medicine, 37(10), 2753-2758..
This includes implementing discharge planning protocols, coordinating with outpatient services for post-ICU care, and providing comprehensive patient education to ensure a smooth transition from the ICU to lower levels of care.
Additionally, leveraging technology like telemedicine platforms for follow-up consultations and remote monitoring or encouraging patients to go through and read their Post-ICU diary entries can help prevent readmissions and facilitate ongoing patient recovery beyond the ICU setting.
Conclusion
Optimizing ICU efficiency is essential not only for reducing costs and maximizing the use of resources but also for making the most out of the expertise and time of ICU staff. However, beyond the financial benefits, efficiency increases both staff and patient satisfaction, enabling better quality of care.
Prioritizing efficiency within the ICU is not just about managing resources—it’s about ensuring the best possible care for patients and creating a supportive and fulfilling work environment for healthcare professionals.