You wake up in a sterile hospital room, disoriented and confused. Machines whir around you, bright lights in you face, and you have no memory of the events that led you here. This is a common experience for ICU survivors, who often struggle with both physical and emotional consequences. Traditionally, medicine has focused on the physical aspects of healing. But what about the stories these patients carry? Narrative medicine offers a powerful tool to help ICU survivors process their experiences and find healing through the power of storytelling.
What is Narrative Medicine?
Narrative medicine is a field that connects traditional medicine and the power of storytelling in healthcare. It emphasizes understanding the patient’s story, them as a person and the context around their medical history.
Here’s how it works:
- Narrative medicine borrows skills from analyzing literature and applies them to patient interactions. It involves recognizing the narrative elements – plot, characters, metaphors – within a patient’s story to foster empathy and understanding between them and the healthcare provider.
- This approach goes beyond simply diagnosing and treating physical symptoms. It delves into the relational and psychological aspects of illness, acknowledging the impact on the whole person.1Charon, R. (2001). Narrative medicine: a model for empathy, reflection, profession, and trust. Jama, 286(15), 1897-1902.
Narrative medicine emphasizes the significance of patients sharing their stories and healthcare providers actively listening to those stories. This not only provides a therapeutic benefit for patients who feel heard and validated, but also enhances the patient-provider relationship.
It complements traditional evidence-based medicine by incorporating the patient’s personal story, empathy, non-verbal communication and contextual understanding of their illness. This integration enhances the clinical encounter and promotes better patient care.2Rosti, G. (2017). Role of narrative-based medicine in proper patient assessment. Supportive Care in Cancer, 25, 3-6.3Charon, R. (2001). Narrative medicine: a model for empathy, reflection, profession, and trust. Jama, 286(15), 1897-1902.
The Impact of Narrative Medicine
Narrative medicine profoundly impacts patient care and clinician well-being by fostering empathy, reflection, professionalism, and trust. Its integration into medical practice is increasingly recognized as a way to humanize healthcare and promote better outcomes for all involved.4DuPerier, E. G. (2023). The Role of Narrative Medicine in Patient Healing and Meaningful Clinical Practice.
Impact on Patient Care
- Shifts focus back to the patient for deeper connection and more comprehensive care
- Recognizes unique patient experiences and perspectives
- Provides a more contextual understanding of illness, leading to better outcomes
- Emphasizes empathy and strong patient-provider relationships
Impact on Clinicians
- Combats burnout and restores meaning in work
- Reminds clinicians of their initial passion for medicine
- Decreases emotional exhaustion through exposure and reflection
- Promotes the development of a resilient and empathetic professional identity
- Teaches critical listening and attention to silenced stories
Narrative Medicine in ICU Recovery
ICU survivors often face a complex journey towards recovery. Apart from the initial physical challenges of regaining strength and mobility, they can also experience:
- Emotional trauma from the frightening and disorienting ICU environment. Patients may have fragmented memories or feelings of anxiety and depression due to their experience.
- Cognitive difficulties like memory problems, difficulty concentrating, and trouble with decision-making.
- Social challenges where reintegrating into daily life and work can be difficult due to physical limitations and emotional distress.
Post-Intensive Care Syndrome (PICS)
Studies5Burdick, K., & Callahan, C. (2020). Sleeping Soundlessly in the Intensive Care Unit. Multimodal Technol. Interact., 4, 6.6Abbas, A., Zayed, N., & Lutfy, S. (2019). Post ICU syndrome among survivors from respiratory critical illness. A prospective study. Egyptian Journal of Bronchology, 13, 505-509.7Wang, S., Hanneman, P., Xu, C., Gao, S., Allen, D., Golovyan, D., Kheir, Y., Fowler, N., Austrom, M., Khan, S., Boustani, M., & Khan, B. (2019). Critical Care Recovery Center: a model of agile implementation in intensive care unit (ICU) survivors. International Psychogeriatrics, 32, 1409 – 1418. show 50% to 75% of survivors experience some form of Post-Intensive Care Syndrome (PICS), a condition characterized by a combination of the above challenges. PICS can significantly impact a person’s quality of life and well-being.
Narrative medicine offers a powerful tool to support ICU recovery by:
- Providing a Platform for Processing Trauma: Sharing their story allows patients to express their experiences and emotions, fostering healing and emotional catharsis.
- Promoting Self-Understanding: Narrating their ICU journey can help patients gain clarity about their experiences and identify areas for improvement, both physically and emotionally.
- Enhancing Communication: By sharing their story with healthcare providers, patients can improve communication and collaboration in their recovery plan.
Narrative medicine empowers ICU survivors to become active participants in their healing process, leading to a more holistic and compassionate approach to recovery.
Practical Narrative Medicine Examples in the ICU Settings
Narrative medicine in ICU settings involves various practical examples that help clinicians build strong connections with patients and families. Here are a few examples:
- Word Clouds: Word Clouds are a visual representation of a patient’s story, created by eliciting words from patients and their families that capture the essence of their experiences and memories.8Vanstone, M., Toledo, F., Clarke, F., Boyle, A., Giacomini, M., Swinton, M., … & Cook, D. (2024). Narrative medicine and death in the ICU: word clouds as a visual legacy. BMJ supportive & palliative care, 14(e1), e634-e641.
- Patient Stories: Sharing patient stories can help clinicians understand the patient’s unique experiences and perspectives. This approach can be particularly valuable in the ICU, where patients are often critically ill and their lives are at risk. By sharing patient stories, clinicians can develop empathy and provide more personalized care.9Facioli, A. M., Amorim, F. F., & de Almeida, K. J. Q. (2012). A model for humanization in critical care. The Permanente Journal, 16(4), 75.
- Reflective Practice: Reflective practice involves clinicians reflecting on their own experiences and emotions to better understand the patient’s story. This approach helps clinicians develop narrative competence, which is the “ability to recognize, absorb, metabolize, interpret, and be moved by the stories of illness”.10Primerano, E., & Alampi, D. (2019). Narrative medicine in intensive care. J Anesth Clin Care, 6, 43.
- Family Meetings: Family meetings are an essential part of narrative medicine in the ICU. These meetings involve clinicians discussing the patient’s condition and treatment options with the family, acknowledging their concerns and emotions, and addressing their needs. This approach helps to promote transparency, trust, and empathy.11Facioli, A. M., Amorim, F. F., & de Almeida, K. J. Q. (2012). A model for humanization in critical care. The Permanente Journal, 16(4), 75.
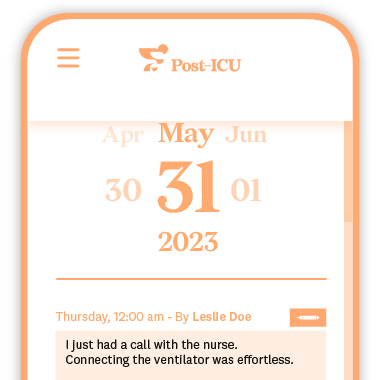
Tools for Narrative Medicine: Post-ICU Diary
The Post-ICU Digital Diary is a valuable tool that utilizes narrative medicine principles to support ICU recovery. Here’s how it empowers patients:
- Processing the ICU Experience: Writing about their time in the ICU or reading about it allows patients to express their thoughts, feelings, and memories and understand what they went through. This process can be cathartic and help them come to terms with a potentially traumatic experience.
- Tracking Progress and Identifying Improvement Areas: The diary functions as a record of the recovery journey. Patients can track their physical, emotional, and cognitive progress over time. By reflecting on entries, they can identify areas that need more focus in their recovery plan.
- Communicating Effectively with Healthcare Professionals: The diary entries can be shared with doctors, nurses, and therapists. This rich narrative provides valuable context about the patient’s experience and can be used to create a more personalized and effective recovery plan.
The Post-ICU Diary is a powerful example of how narrative medicine can be translated into a practical tool for patients and healthcare professionals alike. It fosters self-awareness, facilitates communication, and ultimately empowers ICU survivors to navigate their path to healing.