Burnout syndrome is characterized by emotional exhaustion, depersonalization, and reduced professional efficacy and self-esteem. It affects many healthcare workers, especially those caring for critically ill patients.
In fact, over 50% of critical care health professionals experience burnout.
ICU staff plays a crucial role in patient care, therefore burnout in ICU staff is a critical problem with serious consequences, and hospital leadership needs to take action to prevent and address it. In this article, we’re going to deconstruct the problem by looking at the consequences of burnout, factors that contribute to it, and potential solutions.1Azoulay, E., Lescale, O. Burnout syndrome in healthcare providers: a preventable disease. Intensive Care Med 49, 485–486 (2023).2Moss, M., Good, V. S., Gozal, D., Kleinpell, R., & Sessler, C. N. (2016). A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. American journal of respiratory and critical care medicine, 194(1), 106-113.
Why Is Burnout a Critical Problem for Hospitals
Burnout is associated with increased job turnover, reduced patient satisfaction, and decreased quality of care. Burnout in nurses is linked to lower quality of care, reduced patient satisfaction, increased medical errors, higher healthcare-associated infections, and higher 30-day mortality rates. Burned-out nurses are more likely to make mistakes, be involved in malpractice suits, and have patients who are less likely to follow medical recommendations
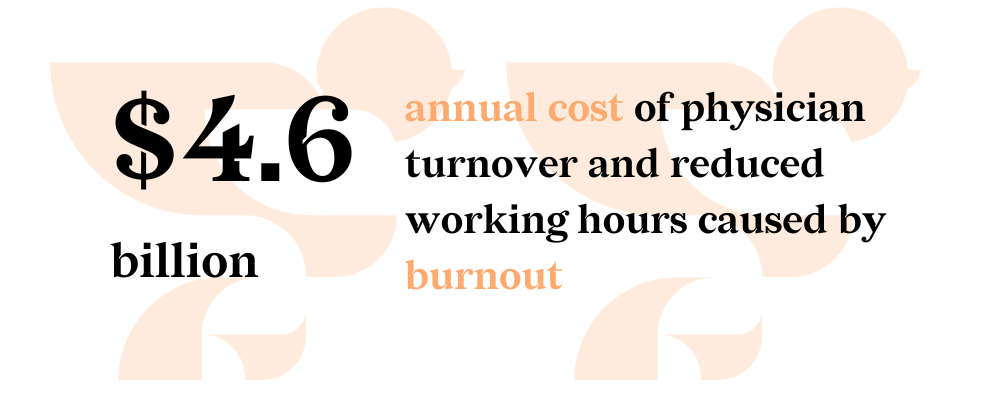
Since burnout syndrome is such a widespread, prevalent issue, it also presents a financial burden.
- A 2019 study estimated the annual cost of physician turnover and reduced working hours caused by burnout to be $4.6 billion in the U.S. alone3Han, S. et al. (2019). Estimating the attributable cost of physician burnout in the United States. Annals of internal medicine, 170(11), 784-790.
- The cost of individual physician turnover is at least $500,0004https://www.mgma.com/mgma-stats/please-don-t-go-ways-to-reduce-physician-turnover
- The cost of individual staff RN turnover is $40,0385https://www.advisory.com/daily-briefing/2022/10/17/nurse-turnover
Given both the financial and human costs, the urgency to alleviate and resolve this problem is apparent. But in order to develop an effective approach, we first need to understand what causes burnout syndrome.
Reasons for Critical Care Providers’ Burnout
The following factors include a combination of organizational, personal, psychological, and contextual factors that affect burnout rates among critical care staff:
- Poor personnel ratios, an excessive workload, and overtime shifts
- Extended workdays, including weekends and nights
- Conflicts and a lack of cooperation among the medical staff
- Ongoing exposure to serious disease, trauma, suffering, and death
- Ethical distress and inability to deliver the necessary quality of care
- Insufficient resiliency and coping strategies
Taking care of these issues will help avoid or lessen burnout’s symptoms. We will give a summary of practical tactics in the next section.
Potential Solutions for Reducing Burnout in the ICU
Addressing Workload and Staffing
Number one strategy on this list is making sure that the ICU is managed well. This means the ICU is organized, with enough staff available to ensure safe staff-to-patient ratios. Alternative scheduling models can also be explored – shorter shifts, more breaks during shifts, shifts that are further apart, etc. Finally, the workflow in the ICU should be streamlined without overburdening staff with administrative tasks or paperwork that could be delegated or reduced.
Enhancing Work-Life Balance
Next, promoting work-life balance is essential. Critical care staff needs to be able and allowed to disconnect from work completely. This entails flexibility on the hospital’s side, providing adequate time off, and showing respect and appreciation for the staff through making it possible for them to live their lives outside the ICU.
Supporting Mental & Emotional Wellbeing
“Give a man a fish and you feed him for a day. Teach him how to fish and you feed him for a lifetime”. Even with a well-organized ICU and a good work-life balance, critical care is stressful. Providing your staff with tools and resources to cope with the stress and build resilience is essential to preserve their mental health. This can entail access to support programs or support people who can recognize and address signs of staff burnout, encouraging open communication, promoting self-care, and providing education.
Enhance ICU Environment and Culture
Through implementing all of the above-mentioned strategies, you can positively influence the ICU culture and make the environment more positive and healthy. A healthy environment fosters better working relationships, creates stronger teams, and helps manage conflict.
Post-ICU Digital Diary Role in Reducing Burnout Syndrome
Post-ICU Digital Diary is a tool that can help you implement patient-centered and family-centered care and also address staff burnout through:
- Strengthening Connections Between Staff, Patients and Families
Easier communication between families and ICU staff builds relationships and rapport
- Humanizing Care
By including photos, videos, and messages, families can share personal stories and updates on the patient’s progress, reminding staff of the individual they are caring for.
- Enhancing Staff Recognition
Families can express gratitude for specific staff interventions and compassionate care, boosting staff morale and sense of accomplishment.
- Reducing Administrative Burden
The diary streamlines communication, potentially reducing the need for repetitive updates and phone calls freeing up time for direct patient care.
Writing in and Navigating an Existing ICU Diary
Watch the ICU Diary DemoSources
- 1Azoulay, E., Lescale, O. Burnout syndrome in healthcare providers: a preventable disease. Intensive Care Med 49, 485–486 (2023).
- 2Moss, M., Good, V. S., Gozal, D., Kleinpell, R., & Sessler, C. N. (2016). A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. American journal of respiratory and critical care medicine, 194(1), 106-113.
- 3Han, S. et al. (2019). Estimating the attributable cost of physician burnout in the United States. Annals of internal medicine, 170(11), 784-790.
- 4https://www.mgma.com/mgma-stats/please-don-t-go-ways-to-reduce-physician-turnover
- 5https://www.advisory.com/daily-briefing/2022/10/17/nurse-turnover