Patient experience is no longer just a feel-good metric – it’s a critical factor that directly impacts a hospital’s bottom line. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) score is a key measure of that experience, surveying patients on their perceptions of the quality of care and experience.
High HCAHPS scores translate to significant financial benefits. Through Value-Based Purchasing (VBP) programs, Medicare and other payers tie a portion of a hospital’s reimbursement to its HCAHPS performance. In simpler terms, higher patient satisfaction leads to higher revenue. Lower patient satisfaction leads to penalties.
But the financial impact goes beyond VBP. Satisfied patients are more likely to return to your hospital for future care, recommend your services to others, and contribute to a positive public reputation – all factors that contribute to a hospital’s long-term success.
This article dives deep into the world of HCAHPS scores, explaining their components and importance. We’ll also explore actionable strategies that hospitals can implement to improve their scores and ensure a positive patient experience throughout their stay.
Understanding HCAHPS
What HCAHPS Measures
HCAHPS doesn’t ask just one question – it explores different areas of a patient’s experience. These categories are like building blocks, each contributing to the overall HCAHPS score equally. Here’s the breakdown of the 8 dimensions:
- Communication with Nurses: This assesses how well nurses explain things clearly, listen to patients’ concerns, and keep them informed about their care.
- Communication with Doctors: Similar to nurses, this dimension focuses on clear explanations, attentiveness to concerns, and keeping patients updated on their care plan by doctors.
- Responsiveness of Hospital Staff: This measures how promptly staff respond to patient requests, such as pain medication or assistance with daily tasks.
- Communication About Medicines: HCAHPS evaluates how well doctors and nurses explain medications to patients, including their purpose, side effects, and proper use.
- Cleanliness and Quietness of Hospital Environment: This dimension assesses patients’ perception of the physical environment, including cleanliness of rooms and overall noise levels.
- Discharge Information: The survey asks if patients received clear and complete instructions about their care after leaving the hospital, including medications, follow-up appointments, and wound care (if applicable).
- Care Transition: This dimension goes beyond discharge information and explores if the hospital effectively facilitates communication with post-acute care providers (e.g., rehab facilities) and offers support services to patients and families during this transition period.
- Overall Rating of Hospital: This captures patients’ general impression of their experience at the hospital, encompassing all the above dimensions.
How HCAHPS Scores are Calculated: A Simplified View
While the official HCAHPS score calculation involves intricate statistics, understanding the core principles can be helpful. Here’s a breakdown with an example:
- Think of HCAHPS as a comprehensive exam. There are eight key areas, like communication with nurses, that are assessed through surveys. Each dimension is worth up to 10 points, with all dimensions worth 80 points. This is the base score.
- Each area is then graded on two factors:
Improvement: This compares the hospital’s performance in that area to its own past performance (e.g., Did communication with nurses improve compared to the baseline period?).
Achievement: This compares the hospital’s performance to a national benchmark (e.g., How does the hospital’s score on communication with nurses stack up against the national average?).
- Hospitals get points for both improvement and achievement, and the higher score for each area is used.
- The consistency score rewards hospitals for consistently exceeding a minimum performance level across all eight HCAHPS dimensions. Think of it like a bonus for well-rounded patient care. It considers two factors:
Your hospital’s lowest-scoring dimension: The further this score is above the national rock-bottom (the “floor” set by the worst performing hospitals in the past), the more points you earn.
The achievement thresholds: These are national benchmarks for each dimension. If all your dimensions are above these thresholds, you get the maximum consistency score.
All these points are combined to create a final HCAHPS score (out of 100).
Example:
Let’s say a hospital’s “Communication with Nurses” score shows a significant improvement compared to the previous year (improvement points). However, the score still falls below the national average (achievement points). In this case, the hospital would receive points for improvement, but not as many for achievement. The final score for “Communication with Nurses” would be based on the higher of these two point values.
Let’s also say the hospital’s lowest score is in “Discharge Information,” but it’s still above the national minimum for that category (the “floor”). Additionally, most of the other dimensions, including communication with doctors, are exceeding the national benchmarks (achievement thresholds). This scenario would result in the hospital receiving some consistency points for the “Discharge Information” score being above the minimum, but likely not the maximum since it’s not exceeding the achievement threshold. However, the high scores in other dimensions would contribute positively to the overall consistency score.
By understanding these core elements, hospitals can identify areas for improvement and develop targeted strategies to achieve a high overall HCAHPS score.
The Importance of HCAHPS for Hospitals
HCAHPS scores aren’t just a reflection of patient experience; they’re a critical factor impacting a hospital’s overall success. Here’s how high HCAHPS scores translate into tangible benefits:
1. Financial Stability through Value-Based Purchasing (VBP)
Remember, HCAHPS scores are a key component of VBP programs implemented by Medicare and other insurers. These programs tie a portion of a hospital’s reimbursement to its patient satisfaction scores. In simpler terms, higher HCAHPS scores mean more money coming into the hospital.
Conversely, low HCAHPS scores can result in significant financial penalties. Think of it as a performance-based bonus system – hospitals that prioritize patient experience are rewarded.
2. Enhanced Public Perception and Reputation
HCAHPS scores are publicly available, allowing patients to compare hospitals based on patient experience. High scores act as a badge of honor, demonstrating a commitment to patient-centered care. This positive reputation attracts new patients seeking a high-quality experience.
Conversely, low scores can damage a hospital’s reputation, leading to negative word-of-mouth and decreased patient trust.
3. Improved Patient Satisfaction and Loyalty
Patients who have a positive experience at a hospital are more likely to be satisfied with their care. High HCAHPS scores indicate a hospital is meeting patient needs, leading to increased satisfaction and loyalty. Satisfied patients are more likely to return for future care and recommend the hospital to others, further strengthening the patient base.
4. Boosted Staff Morale and Recruitment
Working in a hospital with a positive patient experience can be more rewarding for staff. Knowing they’re contributing to a high-quality environment can improve morale and job satisfaction among nurses, doctors, and other healthcare professionals.
High HCAHPS scores can also make a hospital a more attractive workplace, facilitating recruitment and retention of top talent. This creates a positive cycle – a happy and motivated staff leads to better patient care, which in turn contributes to higher HCAHPS scores.
How to Improve HCAHPS Scores
Boosting HCAHPS scores requires a diverse but focused approach. This means having a comprehensive overview of what’s happening in the hospitals and individual departments, collecting and analyzing data to support your findings, and then creating a targeted plan to tackle each problem within each department.
If you’re looking to implement a program to improve HCHAPS scores, start with these steps:
- Leadership mindset needs to align with your goals – good patient experience and HCHAPS scores start from the top. Leadership needs to foster open communication, influence the culture, and hold everyone accountable to stick to the plan and prioritize patient experience.
- Build a knowledge base accessible to the entire staff because without being educated on HCHAPS scores, staff can’t be aware of all the elements that influence them or take proactive steps to change and improve
- Staff needs to have time to focus on patient care. As leadership, it is your responsibility to ensure your staff has time and resources to see each patient as a person, not just a health condition. and not just looking at their health, diagnosis and treatment. It is up to the staff to implement this approach effectively.
- Regularly collect data on patient experience so you can get a complete picture. This requires resources in the form of time and processes set in place to collect data from patients in hospitals but also follow up with them.
- Implement more patient education – patients need to leave the hospital fully informed and aware of their condition, treatments available, support options, etc.
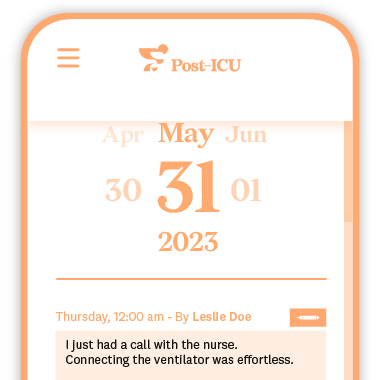
A single tool that can help you implement patient-centered care, free up nurses to focus on patient care, address employee stress rates and collect and act on patient experience data is an ICU diary. While Post-ICU Digital Diary excels as a specialized ICU diary, its core journaling concept could be adapted to enhance patient experiences in various hospital departments.
How Post-ICU Can Help Increase HCAHPS Scores
The journey to recovery doesn’t end when a patient leaves the ICU. Post-ICU, a digital ICU diary specifically designed to support patients and families during and after ICU stays, plays a crucial role in this critical phase. By addressing key areas that directly impact HCAHPS scores, Post-ICU can help hospitals achieve a more positive patient experience.
- Enhanced Communication: Post-ICU provides a secure platform for ongoing communication between patients, families, and healthcare providers. This can address the “Communication with Doctors” and “Communication with Nurses” HCAHPS dimensions. Patients and families can ask questions, share concerns, and receive updates, fostering a sense of transparency and trust.
- Improved Patient Satisfaction: Post-ICU goes beyond basic communication. It offers emotional support, helps families stay engaged in the care process, and represents a proven tool to manage symptoms of Post-Intensive Care Syndrome (PICS). By addressing these often-overlooked aspects of recovery, Post-ICU contributes to a more positive patient experience, directly impacting the “Overall Rating of Hospital Care” HCAHPS dimension.
- Supporting Recovery Throughout the Journey: Post-ICU doesn’t stop at discharge. It continues to offer support and resources as patients transition to home or post-acute care facilities. This promotes a smooth care transition, addressing the “Care Transition” HCAHPS dimension and contributing to a more holistic recovery experience.
- Department Specific Information: While HCAHPS scores provide valuable insight into patient perception of care quality, they don’t pinpoint which specific departments contributed most or least to those perceptions. This is another area where a Post-ICU diary can help. By providing ICU-specific data, the Post-ICU Diary allows hospitals to analyze that data and get insights into their ICU patients’ experience.
Learn more about how Post-ICU can be implemented in your hospital to enhance the patient experience and contribute to achieving high HCAHPS scores.