ICU patient experience has come onto the radar of an increasing number of hospitals over the course of the last year. And for good reason: a better patient experience has been shown to increase clinical outcomes and lower hospital readmissions1Anhang Price, R., Elliott, M. N., Zaslavsky, A. M., Hays, R. D., Lehrman, W. G., Rybowski, L., Edgman-Levitan, S., & Cleary, P. D. (2014). Examining the role of patient experience surveys in measuring health care quality. Medical Care Research and Review, 71(5), 522-554.. As we step into 2024, hospital management and healthcare providers are faced with new challenges and opportunities to enhance the intensive care experience.
This extensive guide will provide you with a 7-step roadmap to improve your ICU experience for patients and their loved ones in 2024. From leveraging technology to fostering effective communication: these steps will help you deliver exceptional care while reducing readmissions and increasing your ICU staff’s job satisfaction.
Why Should You Aim to Improve Intensive Care Experience?
Creating an exceptional patient experience in the Intensive Care Unit (ICU) isn’t just about patients being satisfied with the care they receive. It’s about fostering a positive relationship between professional caregivers, patients, and their loved ones. It’s about empowering patients and families in their vulnerable positions. It’s about adopting a holistic approach to care.
Research shows that a seamless and supportive patient experience contributes to improved patient outcomes, encourages patient loyalty, and enhances the overall reputation of the healthcare facility. So why are some hospitals still struggling to improve their ICU patient experience?
The Most Common Challenges in Improving ICU Patient Experience
While the goal of enhancing patient experience is paramount, hospital staff often encounter numerous challenges in their pursuit of achieving this objective. Research from the World Economic Forum’s “CEOs explain how to respond to the biggest challenges in healthcare” emphasizes the complexities arising from evolving patient needs, technological advancements, and regulatory demands. CEOs from various prominent healthcare institutions, such as Intermountain Healthcare, Home Instead, and Hackensack Meridian Health, emphasize the need for a holistic approach to tackle time constraints in caregiving.
Suggested Solutions to Address Common Challenges
Invest in Innovation
In a recently published article, the World Economic Forum makes important recommendations to counter these common challenges. One of their proposed solutions is to invest in innovation and unlock the full potential of digital tools and technology at scale. Not only should hospitals strive to make current systems work better, but they should also invest in new tools and technologies to really elevate the patient experience. According to the article, only improving current systems is a basic necessity; investing in new tools is where hospitals can truly make a difference for their patients.
Discover how Griffin Hospital increased their ICU patient experience effectively with Post-ICU.
Prioritize Prevention and Early Intervention
Additionally, hospitals should take prevention more seriously. The reason is that prevention, rather than treatments, will benefit all of society. Moreover, hospitals can save great amounts of money. One study2McGarvey, N., Gitlin, M., Fadli, E., & Chung, K. C. (2022). Increased healthcare costs by later stage cancer diagnosis. BMC Health Services Research, 22(1), 1155. found that prevention and earlier intervention can result in medical costs being 3 times lower in the case of cancer, for example.
Foster an Environment that Helps Retain Staff
Another study by McKinsey & Company addresses another major challenge hospitals face: the struggle to hire sufficient staff and retain current staff. McKinsey’s study surveyed more than 700 nurses and more than 150 other healthcare professionals to determine factors that may help them stay in their current job. The most important factors for either staying or leaving their current position are listed in the below graph.
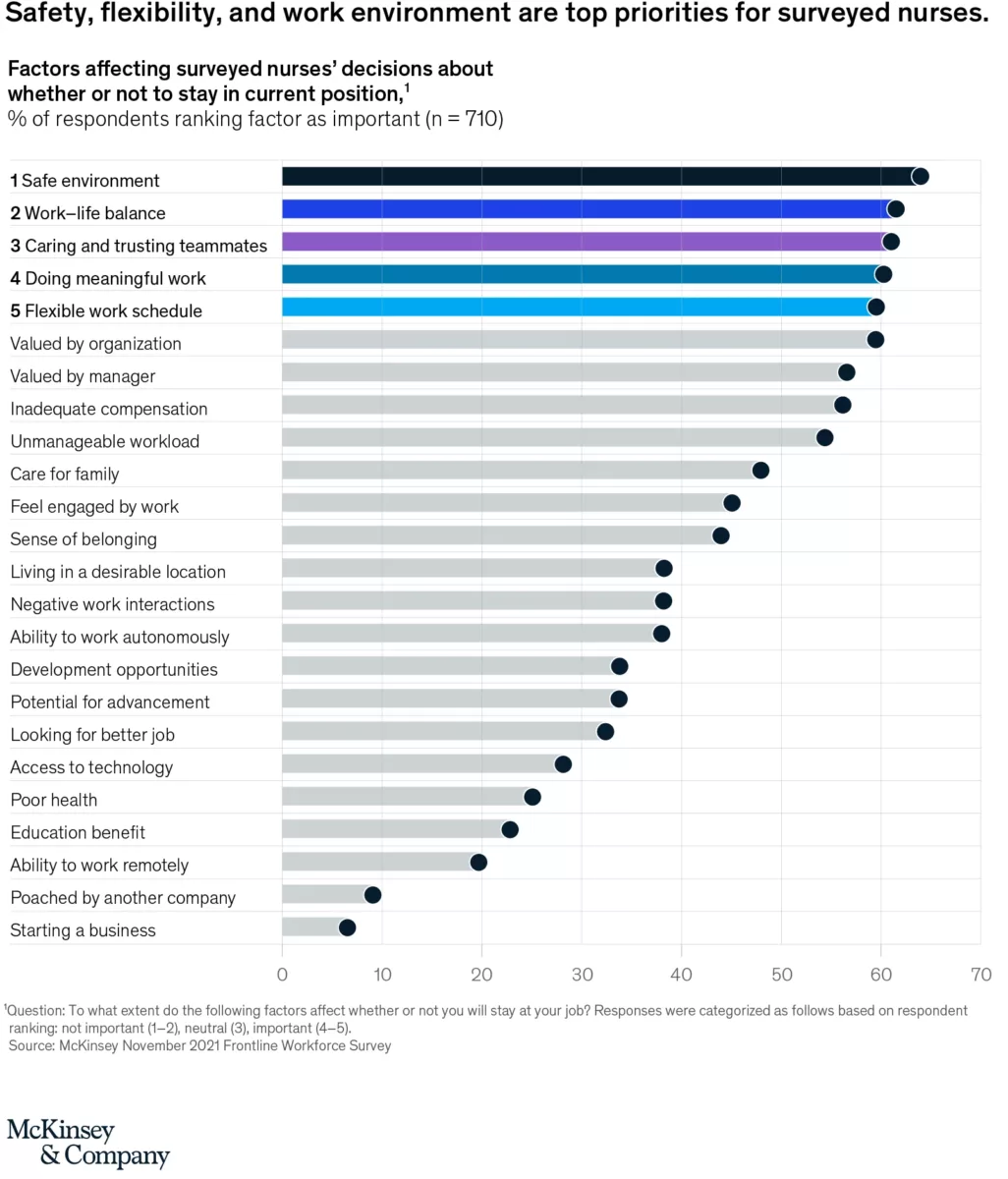
Working in a safe environment proved to be the number one facilitating factor to have nurses and healthcare professionals stay in their current position. Many other of the top factors are, at face value, logical to influence nurses’ willingness to keep their current job.
One facilitator that was especially important for early and midtenured nurses was the ability to care for family of patients. In a study by Dor and Halperin (2022)3Dor, A., & Halperin, O. (2022). Nurses’ job satisfaction and motivation: Patients’ and nurses’ perceptions. Journal of Biosciences and Medicines, 10(6), 121-131., indications have been found to assume that a better patient experience may positively affect nurses’ job satisfaction. This would mean that elevating the patient experience would simultaneously increase the likelihood that staff will want to stay with their current employer.
We have discussed numerous challenges and named possible solutions. But what concrete steps could you take to improve the ICU experience for patients and their loved ones? Follow our 7-step guide below to start taking the ICU experience more seriously and increase your results.
Post-ICU’s 7-Step Guide to Improve ICU Patient and Family Experience
Step 1: Adopting a Holistic Care Mindset
Recognizing that a better ICU experience means caregivers aren’t just taking care of a patient’s body, vitals and symptoms, but also their emotional, social and spiritual health, is the first step. It’s not an optional one, either. If hospitals and staff can’t get behind this idea of wanting to provide care in a holistic manner, it will be very hard to implement any of the below-mentioned steps.
While it’s not necessary to get your whole ICU staff on board with this idea right away, you need to know that at least a large number among the staff share the urgency of adopting a holistic mindset.
If you need help with this, we offer expert advice and training to help you get there. Contact us to discuss your needs.
Step 2: Consider Implementing or Updating Technological Solutions
As was briefly discussed above, many prominent healthcare CEOs agree that investing in technology is crucial to elevate the patient experience. This is true for all departments in hospitals4Skorup, T. E. (2018). Harnessing Technology Innovation to Improve Patient Care. Frontiers of Health Services Management, 34(3), 44-48., but even more so for a better ICU experience. The reason being that ICUs are more hectic and as a result, staff is under more pressure than in other departments.
Leveraging technological solutions can significantly enhance the ICU experience, streamline processes, and also increase ICU caregivers’ job satisfaction. From intuitive health records to a digital ICU diary, implementing technology can streamline processes, improve accessibility, and provide patients and families with a more holistic and convenient ICU experience.
Step 3: Invest in ICU Staff Training and Education
Investing in comprehensive and ongoing staff training programs is crucial. It ensures that professional caregivers possess the necessary skills and knowledge to deliver high-quality medical care.
But apart from staying up-to-date on medical insights, there should also be education for ICU staff concerning the importance of empathetic, holistic care. Recognizing that you’re taking care of a person, instead of a patient, will make a world of difference in terms of the ICU experience.
Consider exploring Post-ICU’s tried-and-true training program and clinical workshops to invest in your staff.
Step 4: Strengthening Family Engagement and Soliciting Feedback
During a patient’s ICU stay, families face significant psychological strain, understanding only about half of the medical information provided5Azoulay, E., Chevret, S., Leleu, G., Pochard, F., Barboteu, M., Adrie, C., … & Schlemmer, B. (2000). Half the families of intensive care unit patients experience inadequate communication with physicians. Critical care medicine, 28(8), 3044-3049.. Proper communication profoundly affects the family’s experience.
Encourage families to provide you with feedback. Professional caregivers should actively involve families (and if possible, patients) in the care they provide when the medical situation allows for it. Of course, not all decisions should be made by families; that would burden them immensely in an already stressful time.
However, involving them in the decision-making process, when it’s appropriate, can empower them and decrease their anxiety levels. Additionally, make sure that processes are in place to regularly implement recommendations in your ICU from patients and families. As a hospital, you’re demonstrating your commitment to a continuous improvement of your ICU experience.
Step 5: Prioritize Timely Communication
The situation can change rapidly on the ICU. Therefore, it’s crucial to communicate in a timely manner with the patient’s loved ones. This will avoid dissatisfaction and frustration. A great way to prioritize communication with the family is by implementing an ICU diary.
Implementing an ICU diary kills two birds with one stone: it is a highly effective tool to increase the patient’s outcomes (read more about Post-Intensive Care Syndrome), and it allows ICU staff to communicate frequently and efficiently with families.
Step 6: Creating a Comfortable and Supportive Environment
Incorporating the 18 domains of discomfort outlined in Figure 1 (modified from Kalfon et al.6Kalfon P, Mimoz O, Auquier P, Loundou A, Gauzit R, Lepape A, Laurens J, Garrigues B, Pottecher T, Mallédant Y. Development and validation of a questionnaire for quantitative assessment of perceived discomforts in critically ill patients. Intensive Care Med. 2010;36(10):1751–8.) should be integrated into daily ICU operations. By comprehensively understanding patients’ experiences and the various factors contributing to their discomfort, the staff can adapt the ICU environment, adjust care practices, and enhance communication with patients effectively.
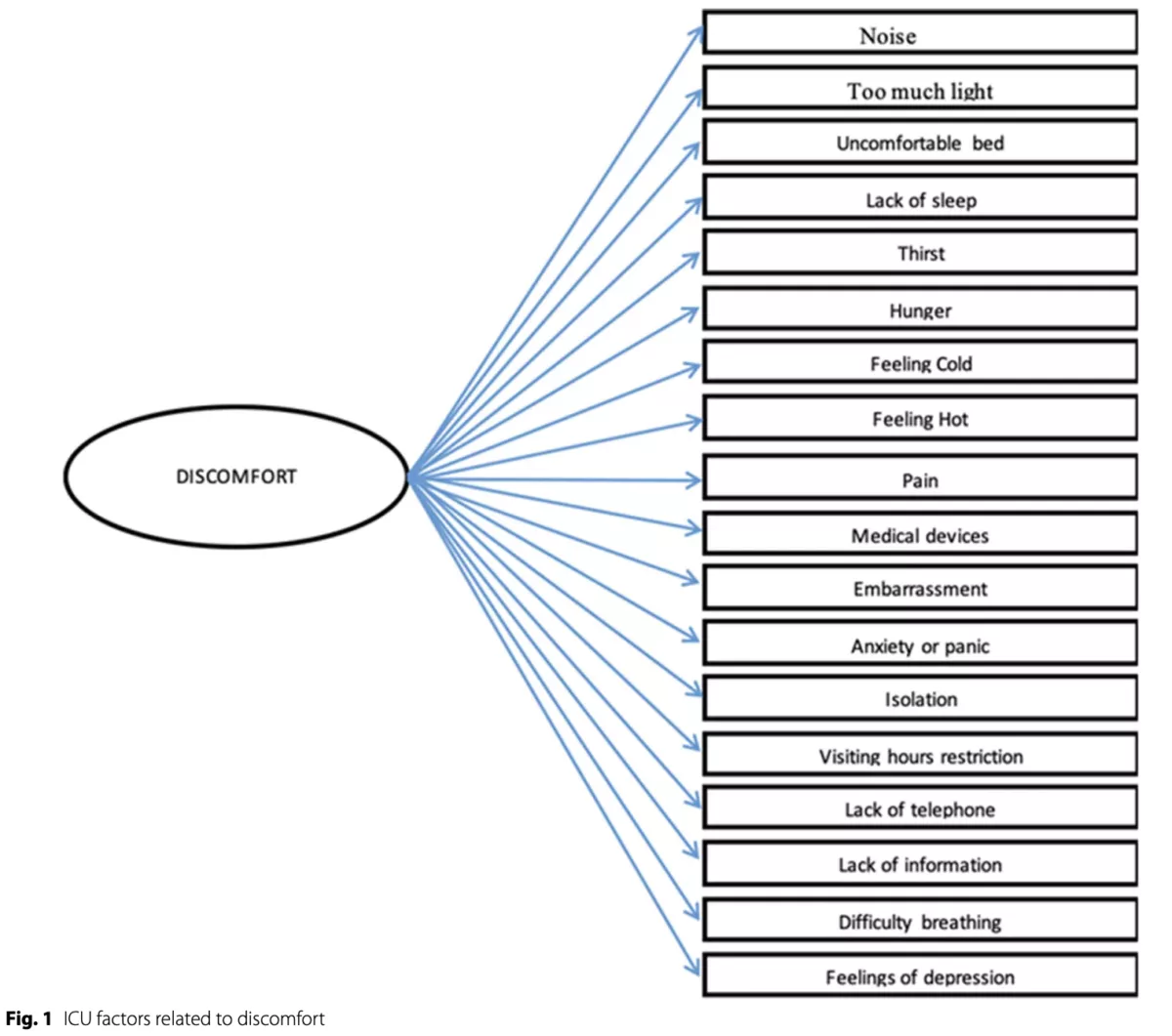
The ICU staff should be mindful of all these types of discomfort and be highly aware of how their actions impacts patients. For example, noise and light are high on the list of irritants7Tronstad, O., Flaws, D., Patterson, S., Holdsworth, R., & Fraser, J. F. (2023). Creating the ICU of the future: patient-centred design to optimise recovery. Critical Care, 27(1), 402. for ICU patients, and their effect can be directly exacerbated by the ICU staff.
Establish a warm and welcoming environment via providing positive distractions (e.g. music), intentional interactions with patients and their families, accessible amenities, etc.
Step 7: Ensuring Continuity of Care and Follow-up Support
Continuity of care stands as a fundamental pillar of effective medical practice8Sharma, G., Freeman, J., Zhang, D., & Goodwin, J. S. (2009). Continuity of care and intensive care unit use at the end of life. Archives of Internal Medicine, 169(1), 81-86. and it’s essential in maintaining a positive patient experience. Offering comprehensive follow-up support, providing access to relevant resources, and fostering ongoing communication can demonstrate a commitment to the long-term well-being and recovery of patients.
Conclusion: A Holistic Approach to Elevate the ICU Patient Experience
Elevating the patient experience isn’t just about providing medical care; it’s about creating a nurturing and supportive environment that prioritizes the physical, emotional, and psychological well-being of patients. By implementing a comprehensive approach that integrates technology, empathetic care, and streamlined processes, professional caregivers can truly revolutionize the patient experience.
FAQs
A positive patient experience can significantly contribute to improved treatment adherence, better health outcomes, and increased patient loyalty to healthcare providers.
Staff empathy plays a crucial role in creating a supportive and compassionate healthcare environment, fostering trust, and building strong patient-provider relationships.
Healthcare facilities can utilize patient feedback to identify areas for improvement, address patient concerns, and implement changes that align with patient preferences and expectations.
Effective strategies for improving communication in healthcare settings include active listening, clear and concise explanations, and the use of empathetic language to ensure patient understanding and comfort. These strategies can be implemented more easily with the help of innovative tools such as the Post-ICU digital diary.
Personalized care demonstrates a deep understanding of a patient's unique needs, fostering a sense of trust, comfort, and individualized support that can significantly enhance the overall patient experience.
Resources
- Anhang Price, R., Elliott, M. N., Zaslavsky, A. M., Hays, R. D., Lehrman, W. G., Rybowski, L., Edgman-Levitan, S., & Cleary, P. D. (2014). Examining the role of patient experience surveys in measuring health care quality. Medical Care Research and Review, 71(5), 522-554.
- Azoulay, E., Chevret, S., Leleu, G., Pochard, F., Barboteu, M., Adrie, C., … & Schlemmer, B. (2000). Half the families of intensive care unit patients experience inadequate communication with physicians. Critical care medicine, 28(8), 3044-3049.
- Berlin, G., Lapointe, M., & Murphy, M. (2022). Surveyed nurses consider leaving direct patient care at elevated rates. McKinsey & Company.
- Dor, A., & Halperin, O. (2022). Nurses’ job satisfaction and motivation: Patients’ and nurses’ perceptions. Journal of Biosciences and Medicines, 10(6), 121-131.
- Kalfon P, Mimoz O, Auquier P, Loundou A, Gauzit R, Lepape A, Laurens J, Garrigues B, Pottecher T, Mallédant Y. Development and validation of a questionnaire for quantitative assessment of perceived discomforts in critically ill patients. Intensive Care Med. 2010;36(10):1751–8.
- Latour, J. M., Kentish-Barnes, N., Jacques, T., Wysocki, M., Azoulay, E., & Metaxa, V. (2022). Improving the intensive care experience from the perspectives of different stakeholders. Critical Care, 26(1), 218.
- Sharma, G., Freeman, J., Zhang, D., & Goodwin, J. S. (2009). Continuity of care and intensive care unit use at the end of life. Archives of Internal Medicine, 169(1), 81-86.
- Skorup, T. E. (2018). Harnessing Technology Innovation to Improve Patient Care. Frontiers of Health Services Management, 34(3), 44-48.
- Tronstad, O., Flaws, D., Patterson, S., Holdsworth, R., & Fraser, J. F. (2023). Creating the ICU of the future: patient-centred design to optimise recovery. Critical Care, 27(1), 402.