Confused, agitated patients. Extended ICU stays. Higher healthcare costs. These aren’t isolated incidents; they’re all potential consequences of a common condition – ICU delirium – a harsh reality for up to 80% of critically ill patients1Girard, T., Pandharipande, P., & Ely, E. (2008). Delirium in the intensive care unit. Critical Care, 12, S3 – S3.. This acute change in mental state, accompanied by inattention and altered cognition, not only creates a stressful environment for patients but also silently erodes your hospital’s bottom line.
However, the good news is that hospitals can play a crucial role in preventing and managing ICU delirium. By implementing proactive measures and innovative tools, such as an ICU diary, you can ensure a better patient experience, improve clinical outcomes, and ultimately, strengthen your hospital’s financial standing. This article dives deep into the evidence-based strategies and resources available to combat ICU delirium.
The Impact of ICU Delirium
ICU Delirium Impact on Hospitals
While the human cost of ICU delirium is significant for patients and their families, the impact on hospitals is equally concerning.
- Increased Healthcare Costs: ICU delirium often leads to prolonged stays, requiring additional ventilator support, medications, and nursing care. This translates to a significant financial burden for hospitals, with studies estimating billions of dollars spent annually due to delirium-related complications.2McDaniel, M., & Brudney, C. (2012). Postoperative delirium: etiology and management. Current Opinion in Critical Care, 18, 372–376.
- Greater Use of Resources: Delirious patients can be more challenging to manage, requiring increased staff time for monitoring, calming agitation, and providing reassurance. This can strain hospital resources and potentially impact the quality of care provided to other patients.
- Potential for Legal Issues: Uncontrolled ICU delirium can increase the risk of falls, self-removal of medical equipment, and other safety hazards, as well as contribute to misdiagnosis or delayed diagnoses, inadequate care, and lack of informed consent. If such incidents result in patient injury, hospitals could face legal repercussions and reputational damage.
ICU Delirium Impact on Patients
The true cost of ICU delirium is of course borne by the patients themselves:
- Increased Length of Stay: Delirium can significantly prolong a patient’s time in the ICU. This not only adds to the emotional and physical stress of hospitalization but also exposes them to additional risks associated with prolonged critical care.3Ely, E., Gautam, S., Margolin, R., Francis, J., May, L., Speroff, T., Truman, B., Dittus, R., Bernard, G., & Inouye, S. (2001). The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Medicine, 27, 1892 – 1900.
- Higher Risk of Mortality: Research suggests a link between ICU delirium and increased mortality rates. The disorientation and confusion associated with delirium can interfere with a patient’s ability to participate in their own care, potentially leading to complications.4Pisani, M., Kong, S., Kasl, S., Murphy, T., Araujo, K., & Ness, P. (2009). Days of delirium are associated with 1-year mortality in an older intensive care unit population.. American journal of respiratory and critical care medicine, 180 11, 1092-7 . 5Ely, E. W., Shintani, A., Truman, B., Speroff, T., Gordon, S. M., Harrell Jr, F. E., … & Dittus, R. S. (2004). Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. Jama, 291(14), 1753-1762.
- Cognitive Decline and Long-Term Functional Impairment: One of the most concerning aspects of ICU delirium is its potential to cause long-term cognitive decline. Patients can experience memory problems, difficulty concentrating, and a decline in their ability to perform everyday activities.6Girard, T. D., Jackson, J. C., Pandharipande, P. P., Pun, B. T., Thompson, J. L., Shintani, A. K., … & Ely, E. W. (2010). Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Critical care medicine, 38(7), 1513-1520.7Goldberg, T., Chen, C., Wang, Y., Jung, E., Swanson, A., Ing, C., García, P., Whittington, R., & Moitra, V. (2020). Association of Delirium With Long-term Cognitive Decline: A Meta-analysis. JAMA neurology.
- Psychological Distress: The confusion and disorientation associated with delirium can lead to fear and a feeling of isolation for patients. They may experience anxiety, and depression, further hindering their recovery process.
The impact ICU delirium has on patients, hospitals and critical care staff led to the development of preventative and management strategies outlined below.
Strategies for Reducing ICU Delirium Occurrence and Impact
Preventative Non-Pharmacological Strategies
ICU delirium is not an inevitable consequence of critical illness. Hospitals can significantly reduce its incidence by implementing the following strategies:
Orientation Strategies
- Provide Visual and Hearing Aids: Ensure patients have access to eyeglasses and hearing aids to improve their ability to process information and stay oriented.
- Encourage Communication and Reorientation: Regularly engage patients in conversation, reminding them of their name, location, and date and time. Use simple language and repeat information as needed.
- Familiar Objects: Surround patients with familiar items from home, such as pictures, blankets, or a favorite stuffed animal, to create a sense of comfort and security.
- Consistent Staff: Whenever possible, try to assign the same nurses to care for a patient to minimize confusion and promote trust.
- Family Engagement and Empowerment: Include families in the care plan, provide them with education about ICU delirium, and encourage their presence at the bedside. Having a familiar face can be calming and reassuring for patients.
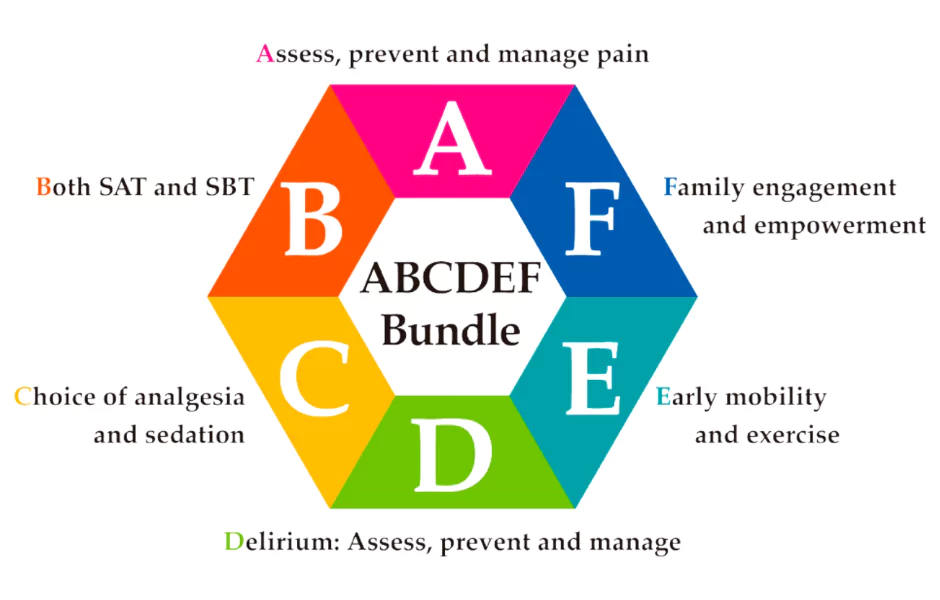
The ABCDEF Bundle
This evidence-based protocol reduces delirium and coma days by 25% to 50%8SCCM: ICU liberation bundle (A-F). Society of Critical Care Medicine (SCCM). (n.d.). https://www.sccm.org/iculiberation/abcdef-bundles. It outlines six key areas for proactive management and addresses various factors that can contribute to delirium, promoting a more alert and oriented state for patients.
Optimizing Environmental Conditions
Maintaining appropriate brightness levels, and a quiet environment with a regular sleep-wake cycle helps promote orientation and reduce sensory overload. 9Hashemighouchani, H., Cupka, J., Lipori, J., Ruppert, M. M., Ingersent, E., Ozrazgat-Baslanti, T., … & Bihorac, A. (2020). The impact of environmental risk factors on delirium and benefits of noise and light modifications: a scoping review. medRxiv, 2020-05.
Cognitive Stimulation
Simple activities like word puzzles or picture recognition can help stimulate cognitive function and prevent mental decline.10Parker, A. M., Aldabain, L., Akhlaghi, N., Glover, M., Yost, S., Velaetis, M., … & Needham, D. M. (2021). Cognitive stimulation in an intensive care unit: a qualitative evaluation of barriers to and facilitators of implementation. Critical care nurse, 41(2), 51-60.
Promote Early Mobilization
Encourage early physical activity and exercise to improve circulation, oxygenation, and cognitive function. This can involve simple activities like sitting up in bed or assisted walking.11Nydahl, P., Jeitziner, M. M., Vater, V., Sivarajah, S., Howroyd, F., McWilliams, D., & Osterbrink, J. (2023). Early mobilisation for prevention and treatment of delirium in critically ill patients: Systematic review and meta-analysis. Intensive and Critical Care Nursing, 74, 103334.
Music Therapy
Consider incorporating music therapy based on patient preferences. Soothing music can promote relaxation and reduce agitation in some patients.12Golubovic, J., Neerland, B. E., Aune, D., & Baker, F. A. (2022). Music interventions and delirium in adults: a systematic literature review and meta-analysis. Brain Sciences, 12(5), 568.
Oxygen Saturation Monitoring
Closely monitor blood oxygen saturation levels and ensure they remain above 90% to prevent hypoxia, which can contribute to delirium.
Addressing Underlying Conditions
Identifying and treating underlying medical conditions such as infections or electrolyte imbalances that can contribute to delirium.
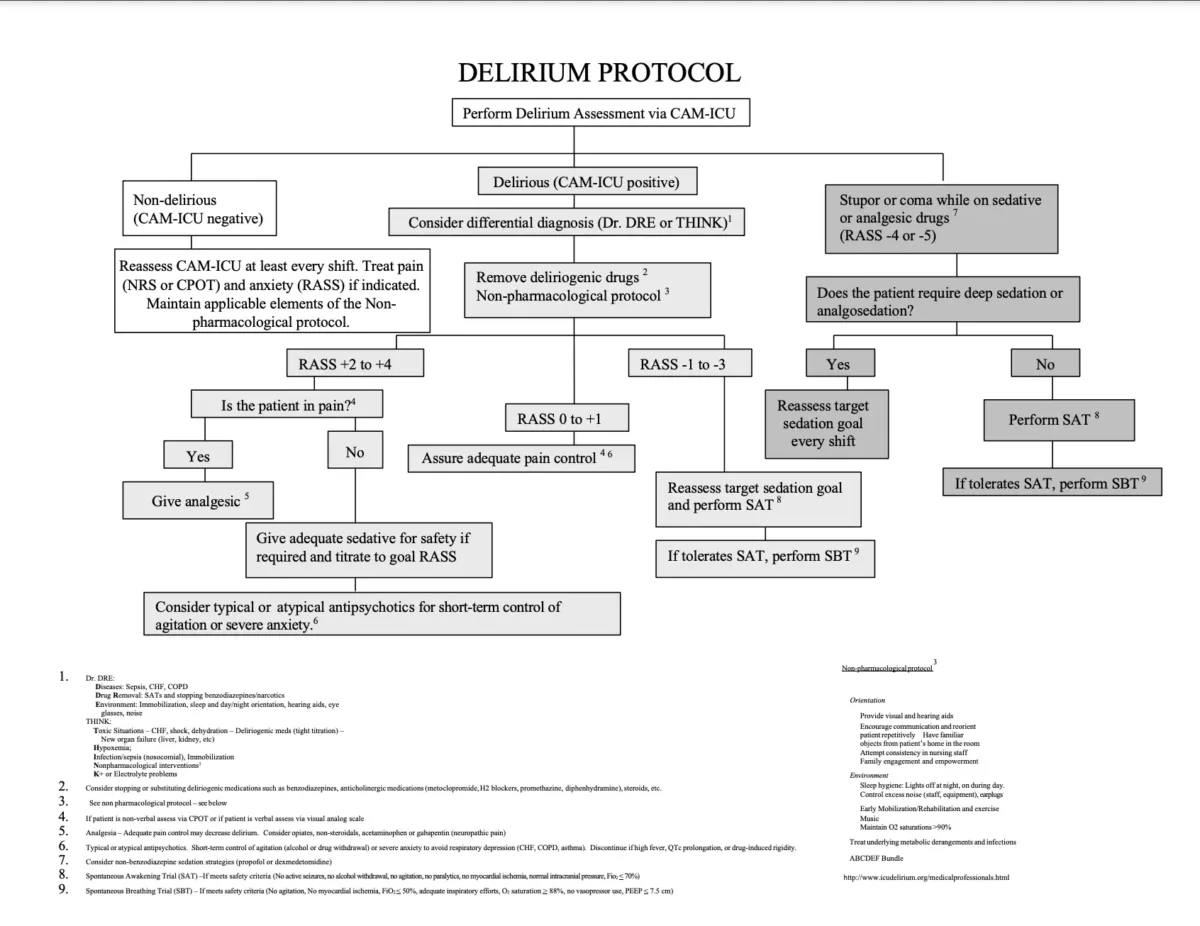
Pharmacological Management Strategies
While prevention is key, some patients will still develop ICU delirium. In such cases, it’s crucial to implement effective management strategies to minimize the impact on patients and support recovery. Here’s what hospitals and ICU staff can do:
- Medication Review: Certain medications might contribute to developing or worsening delirium symptoms. ICU clinicians can review the medications and decide whether to reduce doses or eliminate them.
- Minimize Sedatives and Analgesics: Overuse of sedatives and pain medications, particularly benzodiazepines and narcotics, can worsen cognitive function in patients already experiencing delirium.
- Non-pharmacological interventions – The same non-pharmacological interventions to prevent delirium can be used to manage it and reduce symptoms.
- Consider Antipsychotics: If non-pharmacological interventions prove insufficient, healthcare professionals may consider using antipsychotic medications like haloperidol. However, the use of these medications should be a last resort, and the dose should be started at the lowest level effective for symptom control.
The Role of Post-ICU Digital Diary in ICU Delirium Management
While the strategies mentioned above form the core of ICU delirium management, innovative tools like Post-ICU Digital Diary can offer additional support. This digital diary is made specifically for patients recovering from critical illness and has features that can potentially benefit delirium management in several ways:
- Post-ICU diary provides a record of events during the patient’s ICU stay, written by family, friends, and critical care staff. This can help fill memory gaps and orient the patient to what happened during periods of delirium or unconsciousness. This can reduce the development of post-traumatic stress disorder (PTSD) and other psychological issues after ICU discharge
- The diary is written in everyday language by nurses and family members, describing the patient’s situation and progress. Reading the diary can support the patient’s coping and understanding of their critical illness experience
- Post-ICU diary also functions as a communication tool, allowing patients to discuss their different experiences and views of their illness with family and healthcare providers. This can help process emotions and gain insight into their delirium episode
- Research has shown that ICU diaries are associated with a lower risk of depression and better quality of life in ICU survivors.
Important Note: Post-ICU diary is not a replacement for the core management strategies outlined earlier. However, its features can complement these strategies and offer valuable tools for supporting patients and families while potentially aiding in the early detection and management of ICU delirium.
Conclusion
Hospitals have a critical role to play in preventing ICU delirium. By adopting evidence-based strategies like the ABCDEF Bundle and considering innovative tools like Post-ICU digital diary, healthcare providers can create a culture of delirium prevention, optimize patient care, and ensure a more successful outcome for everyone involved.