Effective communication in the ICU significantly impacts family satisfaction and the overall quality of care. Families express a strong need for timely, honest, and understandable information regarding their loved one’s condition. Research indicates that poor communication is a leading source of dissatisfaction among families, with studies showing that as many as 30% of family members1Baker, R., Wu, A. W., Teno, J. M., Kreling, B., Damiano, A. M., Rubin, H. R., … & Lynn, J. (2000). Family satisfaction with end‐of‐life care in seriously ill hospitalized adults. Journal of the American Geriatrics Society, 48(S1), S61-S69. report being unhappy with the communication they receive from healthcare providers. Furthermore, effective communication can help mitigate psychological distress, reduce anxiety, and improve the family’s ability to make informed decisions regarding treatment options.2Alhussaini, A. (2021). Improve communicating uncertainty in intensive care unit with patient and family (ICU-PF). Cureus, 13(12).3Jones, M. (2023). Improving family communication in critical care. Canadian Journal of Critical Care Nursing, 34(1).
Barriers to Effective Communication
Understanding the barriers to effective communication is crucial for developing strategies to overcome them. Key barriers include:
- Health Literacy: Many family members struggle to understand complex medical terminology and concepts, which can lead to confusion and frustration.
- Cultural Diversity: Differences in language, cultural values, and beliefs can hinder effective communication.
- Environmental Factors: The ICU environment is often busy and noisy, making it difficult for sensitive discussions to take place. The stress of the setting can further complicate communication efforts.
Strategies for Improving Communication in the ICU
Family-centered Rounds and Structured Family Meetings
Family-centered rounds involve including family members in daily rounds, allowing them to ask questions and receive updates directly from the healthcare team. In contrast, structured family meetings provide a dedicated time for in-depth discussions about the patient’s condition and care plan. Both approaches are important because both the healthcare providers and the families get time and space to speak and ask questions.
Communication Frameworks
Using established communication frameworks can improve communication with families in the ICU. Frameworks such as the READY framework, Integrated Communication Framework, and Facilitated Sensemaking Model provide structured approaches to ensure that communication is clear, empathetic, and responsive to family needs.
Components of the READY Framework
- Right Language: using clear, jargon-free language that is easily understood
- Environment: creating a supportive and private space for discussions, minimizing distractions and ensuring comfort
- Assessment of Families’ Readiness to Communicate: evaluating whether family members are prepared to engage in discussions and receive important information
- Do Your Preparation: coming to discussions well-prepared with relevant information about the patient’s condition, treatment options, and potential outcomes
- You Have the Opportunity to Deliver Different Types of Information: recognizing that families may require various types of information, including clinical updates, emotional support, and practical guidance4Mackie, B. R., Mitchell, M., & Schults, J. (2021). Application of the READY framework supports effective communication between health care providers and family members in intensive care. Australian Critical Care, 34(3), 296-299.
Components of the Integrated Communication Framework
- Multimodal Communication Platforms: The framework recognizes that no single communication method is sufficient to meet the diverse needs of families. Instead, it integrates various platforms, including family-centered rounds, bedside or telephone updates, electronic family portals, etc.
- Goals of Communication: The framework outlines five primary goals that clinician-family communication should achieve:
- Establishing trust
- Providing emotional support
- Conveying clinical information
- Understanding the patient as a person
- Facilitating careful decision-making
- Flexibility and Responsiveness: The need for flexibility in communication is emphasized. It allows HCPs to adapt their approach based on the evolving needs of families, ensuring that communication is timely and relevant throughout the patient’s ICU stay.
- Structured Family Meetings: While informal updates are important, the framework also highlights the ongoing relevance of the structured family meetings we mentioned. 5Seaman, J. B., Arnold, R. M., Scheunemann, L. P., & White, D. B. (2017). An integrated framework for effective and efficient communication with families in the adult intensive care unit. Annals of the American Thoracic Society, 14(6), 1015-1020.
By using these or other available structured communication models, healthcare providers have something similar to a playbook for communication, ensuring that the complexities of ICU communication are considered and the best approach is used with families.
Written Materials
Providing written materials that explain medical conditions, treatment options, and care processes can help bridge the gap in understanding. The shock of a loved one being critically ill has a profound effect on family members and some of them might not be capable of taking in and processing information delivered orally. Many of them will remember only parts of conversations. Having everything in a written form for them to go back to will help them feel supported and informed.
ICU Diaries
ICU diaries allow families to document their experiences and the patient’s progress, serving as a tool for reflection and communication with the healthcare team. The healthcare team can also contribute by providing additional, non-medical context to the patient’s ICU stay. While ICU diaries have significant non-communication-related benefits for everyone involved, they also can act as a communication channel, especially when in digital form.
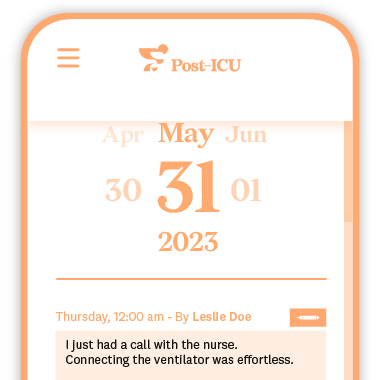
The Post-ICU Digital Diary is a digital ICU diary that can be accessed by family members from anywhere, allowing them 24/7 access to entries and updates, even from home. ICU staff often note down small milestones for the patient, explain what’s happening around the patient at various times, and add encouraging words for both the patient and the family. All of this can be accessed by family and friends at any time, helping them feel better informed, regularly updated, and more in control of the situation.

Emotional Support Techniques
Training healthcare providers in effective communication techniques is crucial. This includes education on using communication frameworks, active listening skills, and cultural competency. Language training can also be beneficial in addressing the needs of diverse populations.
HCP Training
Employing emotional support techniques, such as active listening, empathy, and validation, can improve the quality of interactions with families. Encouraging family narratives allows them to express their concerns and feelings, fostering a supportive environment. A tool such as an ICU diary can also be helpful here.
Organizational Policies and Resources
Hospitals and leadership need to prioritize communication in the ICU. Organizational support is crucial for implementing and ensuring the effectiveness of any of the previously mentioned strategies. It starts by providing foundational resources for successful communication—time and space. This includes allocating time for family meetings, creating quiet spaces for discussions, and providing translation services when necessary. It also involves ensuring sufficient staffing and a workflow that allows time for meaningful communication, so families are not rushed through or dismissed.
Final Thoughts
In the 21st century, with the development of various digital tools, communication should not be a problem. It has never been easier to deliver timely, relevant updates to the families of ICU patients. While human-to-human contact remains the most important form of interaction, many updates can be delivered digitally, which families often prefer over receiving no updates at all. Hospitals should explore solutions to implement in ICUs that enhance communication, fostering stronger relationships and building trust through better communication.