Unplanned readmissions to the intensive care unit are a major concern within healthcare systems. Studies indicate that around 10% of patients discharged from an ICU in developed countries get readmitted during the same hospital stay1Rosenberg, A. L., & Watts, C. (2000). Patients readmitted to ICUs: a systematic review of risk factors and outcomes. Chest, 118(2), 492-502.. These readmissions are not only a financial burden but are also associated with poorer patient outcomes, including increased length of stay, higher mortality rates, and a greater risk of complications2Wong, E. G., Parker, A. M., Leung, D. G., Brigham, E. P., & Arbaje, A. I. (2016). Association of severity of illness and intensive care unit readmission: A systematic review. Heart & Lung, 45(1), 3-9.. This article explores the impact of ICU readmissions on hospital’s bottom line and patient outcomes, as well as a series of proactive strategies for reducing readmissions to the ICU.
The Importance of Reducing Readmissions to the ICU
Reducing ICU readmissions carries significant weight for both hospitals and patients. From a financial standpoint, it’s a major drain on resources. Around 2,300 US hospitals faced penalties in 2023 for excessive readmissions within 30 days of discharge, translating to a loss of a portion of their Medicare revenue. Beyond these penalties, each readmission incurs additional costs for follow-up care.
But the impact extends far beyond finances. Each readmission exposes patients to a greater risk of complications and even mortality, as well as decreased quality of life and satisfaction. The emotional and mental toll on patients and their families can’t be overlooked either.
A commitment to reducing ICU readmissions isn’t just about economic benefits – it’s also about optimizing patient outcomes and ensuring a smoother, less stressful recovery journey for everyone involved.
Identifying High Risk Patients
Identifying patients at high risk for ICU readmission early is an important proactive and preventative step in reducing ICU admissions.
By analyzing factors like disease progression, comorbidities, and previous hospitalizations, healthcare providers can develop a risk score for each patient. This score can then be used to prioritize interventions and allocate resources to those most likely to benefit.
Beyond traditional medical factors, social determinants of health, such as socioeconomic status and access to healthcare, also play a significant role in readmission risk3Hu, J., Gonsahn, M., & Nerenz, D. (2014). Socioeconomic status and readmissions: evidence from an urban teaching hospital.. Health affairs, 33 5, 778-85.
Here’s a specific example to illustrate the point:
Literature suggests4Grottenthaler, C., & Reese, C. (2012, December). REDUCING ICU READMISSIONS. In Critical Care Medicine (Vol. 40, No. 12, pp. U36-U36). 530 WALNUT ST, PHILADELPHIA, PA 19106-3621 USA: LIPPINCOTT WILLIAMS & WILKINS that respiratory failure is the leading cause of ICU readmission, accounting for nearly half of all cases. By implementing an assessment checklist and risk score specifically focused on respiratory function, healthcare teams can identify high-risk patients within 72 hours of discharge who might experience complications. This early identification allows for targeted interventions, potentially reducing the rate of ICU readmissions for these patients.
Optimize Transitional Care
Transitioning from the ICU to the next stage of care is crucial for a successful recovery and
preventing readmissions. This involves:
- developing clear and concise discharge instructions that are easy for patients and families to understand
- early follow-up appointments with primary care physicians or dedicated follow-up nurses to ensure continuity of care and allow for timely identification of any issues
- strong communication between ICU teams and post-discharge to create a collaborative environment where all parties are working towards the patient’s successful recovery.
By bridging these potential gaps, hospitals can significantly reduce the risk of complications and readmissions.
Promoting Medication Adherence
Studies5Rosen, O. Z., Fridman, R., Rosen, B. T., Shane, R., & Pevnick, J. M. (2017). Medication adherence as a predictor of 30-day hospital readmissions. Patient preference and adherence, 801-810. have shown a clear link between low medication adherence and an increased risk of returning to the ICU. By educating patients on the importance of their medications, their potential side effects, and exploring medication management tools like pillboxes or reminders, healthcare teams can empower patients to take an active role in their recovery and reduce the likelihood of complications that might necessitate readmission.
Preventing Hospital-Acquired Infections
Patients in the ICU are especially vulnerable to hospital-acquired infections due to factors like weakened immune systems, invasive procedures, and the use of catheters and ventilators.
Adherence to sterile procedures and responsible antibiotic use are powerful tools in the fight against HAIs.6Jing, W. (2007). Clinical Analysis of Hospital Acquired Infection in Intensive Care Unit. Journal of Internal Intensive Medicine. By implementing strict hand hygiene protocols, utilizing appropriate catheter and ventilator management techniques, and encouraging early mobilization of ICU patients whenever possible, healthcare teams can significantly reduce the risk of HAIs and the associated risk of readmission.
Strengthening Patient and Family Engagement
Strong patient and family engagement has been shown to reduce the length of stay in the ICU and improve adherence to ICU recovery instructions, ultimately leading to lower readmission rates.
Hospitals can achieve this by educating the families on the patient’s condition, recovery process, and potential complications, as well as empowering them to advocate for their loved ones.
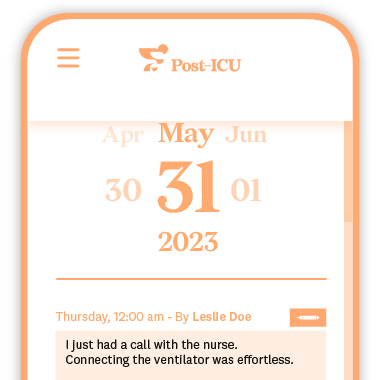
The use of technology in the ICU can also help foster family engagement – specifically in ICU diaries. The Post-ICU digital diary stands as a scientifically validated tool for enhancing family engagement. This tool allows families to journal their experiences, communicate with staff, and stay updated on the patient’s progress. For patients, the diary can also help piece together lost time during their ICU stay, potentially reducing the occurrence of post-ICU syndrome (PICS), a frequent and challenging consequence of critical illness.
By prioritizing patient and family engagement through these strategies, hospitals can foster a supportive environment that promotes successful recovery and reduces the likelihood of ICU readmissions.
Improved Patient Outcomes and a Healthier Bottom Line
Reducing readmissions to the ICU is a win-win situation for everyone involved. Hospitals not only improve their financial standing but, more importantly, ensure a smoother recovery journey and better overall outcomes for their patients.