In most cases, ICU stays are a traumatic experience for both the patients and their families. This type of trauma can leave lasting consequences. For patients, these consequences can be physical, psychological, cognitive, and social. With the development and improvement of ICU care, treatments and healthcare overall, more people are now able to recover after their ICU stays. However, this also means that more people are experiencing the aftermath of ICU trauma. It is important to understand what happens after a patient is discharged from the ICU to better prepare and be able to support them. This article will explore that in detail.
ICU to Ward Transition
Typically, ICU patients first get transferred from the ICU to the general ward. This happens when the patient no longer needs 24/7 constant monitoring and intensive nursing care. Transferring to the ward is seen as a sign of recovery. The patient is no longer critically ill. However, this transition must be done carefully and in an organized manner because it is a vulnerable time for the patient. When patients are being transferred they may1Herbst, L. A., Desai, S., Benscoter, D., Jerardi, K., Meier, K. A., Statile, A. M., & White, C. M. (2018). Going back to the ward—transitioning care back to the ward team. Translational pediatrics, 7(4), 314.:
- Experience post-intensive care syndrome
- Feel insecure or lonely due to the change of setting and the care team
- Feel shock due to the nature of the situation, change in the daily routine, requirement to use new technologies to manage their condition (if applicable)
During and after transfer, patients are also at a higher risk of medical errors. As mentioned, all of these can be mitigated by safe, complete and timely patient handoff and medication reconciliation.
Once the transition is completed, the patient will stay in the ward while they require ongoing care, physical therapy or rehabilitation. Several differences can be noted compared to the ICU: General wards typically have a lower nurse to patient ratio, more beds per room and the role of the family often changes from part of the care team to visitors, which can also be a source of stress.
Ward to Home
As the patient stabilizes, the care team will start assessing if the patient is ready to be discharged. Patient discharge should always be carefully planned, and both the patients and the families should receive enough education and support to be able to provide necessary care at home. This includes instructions for managing certain health conditions, medications, follow-up appointments and how to recognize signs of complications or decline.
The role of the family is especially important at this stage. As mentioned, ICU patients suffer a host of consequences after the ICU and they frequently need additional support even after discharge. The role of the family as part of the care team starts in the ICU, where they learn and participate in the care of their loved one. A tool such as an ICU diary can help involve the family and keep them engaged.
When the patient is transferred to the ward and later discharged, the role of the family changes slightly but it’s still very important. The family can ensure that the patient follows doctor orders, makes the follow up appointments and stays compliant. This can decrease the chance of being readmitted to the hospital or even the ICU.
Follow Up Care after the ICU
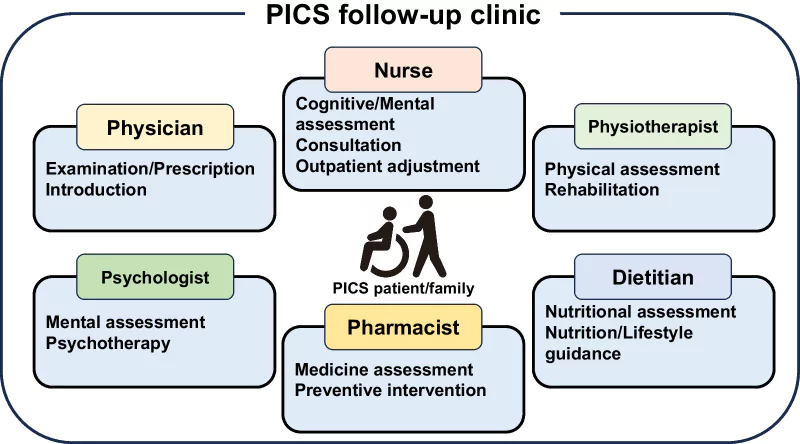
In the United States, ICU follow-up care typically involves PICS follow-up clinics, telemedicine-based interventions, and support resources.2Nakanishi, N., Liu, K., Hatakeyama, J., Kawauchi, A., Yoshida, M., Sumita, H., … & Nakamura, K. (2024). Post-intensive care syndrome follow-up system after hospital discharge: a narrative review. Journal of Intensive Care, 12(1), 2.
PICS follow-up clinics consist of multidisciplinary teams that provide monitoring and support for various types of issues ICU patients might have during recovery. There is no scientifically supported recommendation on how soon after the discharge should the patient be assessed. Some studies suggest 1-3 months after discharge3Cuthbertson, B. H., Rattray, J., Campbell, M. K., Gager, M., Roughton, S., Smith, A., … & Waldmann, C. (2009). The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. Bmj, 339., while SCCM recommends assessment as soon as 2-4 weeks after discharge4Mikkelsen, M. E., Still, M., Anderson, B. J., Bienvenu, O. J., Brodsky, M. B., Brummel, N., … & Sevin, C. M. (2020). Society of Critical Care Medicine’s international consensus conference on prediction and identification of long-term impairments after critical illness. Critical care medicine, 48(11), 1670-1679. for high-risk patients, and a follow-up assessment 6-12 after discharge. The assessments need to be conducted every few months. If the patient is unable to visit the clinic, telephone or email-based assessments are frequently an option.
FIND A CLINIC AND OTHER SUPPORT RESOURCES: A Directory of PostICU Clinics
The effectiveness of PICS follow up clinics as well as the recommendation for optimal use of these resources require further research.
Nakanishi, N., Liu, K., Hatakeyama, J., Kawauchi, A., Yoshida, M., Sumita, H., … & Nakamura, K. (2024). Post-intensive care syndrome follow-up system after hospital discharge: a narrative review. Journal of Intensive Care, 12(1), 2.
Common Challenges After Leaving the ICU
After leaving the ICU, both patients and families may experience the consequences of this trauma. While family consequences tend to be psychological, patients experience a wide range of negative effects and symptoms, collectively known as Post-Intensive Care Syndrome (PICS). Here’s what you can expect:
- ICU-acquired weakness which is physical weakness affecting muscles, balance, daily activities and recovery
- Cognitive dysfunction that affects memory, problem solving, attention
- Emotional and psychological effects such as anxiety, depression, PTSD
- Problems with sleep after sleep pattern disruption in the ICU
- Problems with eating, poor appetite, difficulty swallowing
Unfortunately, a large percentage of ICU patients will experience these symptoms during their recovery.
Post-ICU Digital Diary: A Validated Tool for PICS prevention
An ICU diary is a validated intervention that alleviates or mitigates symptoms of PICS for patients and families alike. Here’s how it works:
- Journaling helps process the trauma. While the patient is in the ICU, the family and critical care staff contribute to a journal, creating a shared narrative and giving context to the medical information.
- Through journaling, families are engaged in the care of the patient, while they also process their own feelings and express their thoughts and support for the patient
- The patient’s experience and memory in the ICU is often fragmented or even altered as a consequence of ICU delirium. The shared narrative, the story that was written about and for the patient while in the ICU can help them piece together what happened, regain the feeling of control, and cope with the trauma while they are recovering.
- The story in the diary can make up for the lost time, show to patients the support and care they received, and have an overall positive impact on their recovery.
The Post-ICU Digital Diary is the only digital solution for ICUs. It protects patients’ privacy, makes journaling easy and easily available to patients and families.
Writing in and Navigating an Existing ICU Diary
Watch the ICU Diary DemoSources
- 1Herbst, L. A., Desai, S., Benscoter, D., Jerardi, K., Meier, K. A., Statile, A. M., & White, C. M. (2018). Going back to the ward—transitioning care back to the ward team. Translational pediatrics, 7(4), 314.
- 2Nakanishi, N., Liu, K., Hatakeyama, J., Kawauchi, A., Yoshida, M., Sumita, H., … & Nakamura, K. (2024). Post-intensive care syndrome follow-up system after hospital discharge: a narrative review. Journal of Intensive Care, 12(1), 2.
- 3Cuthbertson, B. H., Rattray, J., Campbell, M. K., Gager, M., Roughton, S., Smith, A., … & Waldmann, C. (2009). The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. Bmj, 339.
- 4Mikkelsen, M. E., Still, M., Anderson, B. J., Bienvenu, O. J., Brodsky, M. B., Brummel, N., … & Sevin, C. M. (2020). Society of Critical Care Medicine’s international consensus conference on prediction and identification of long-term impairments after critical illness. Critical care medicine, 48(11), 1670-1679.